-
Services
-
At Audiology-Hearing Aid Associates of SE Texas, we provide full-service care for our patients' hearing. We maintain qualified doctors on staff specializing in diagnosis and treatment of virtually any hearing-related difficulty, from audiological testing to hearing-aid fitting and more.
Our Services include:
-
Diagnostic Audiological Testing
-
Hearing Aid Evaluations & Fittings
-
Hearing Aid Repairs - All Makes & Models
-
Batteries & Supplies
-
Central Auditory Testing
-
Swim & Noise Plugs
-
Musician's Ear Plugs
-
Brainstem Auditory Testing
-
ENG Testing (dizziness)
-
Cerumen (wax) Removal
-
Otoacoustic Emissions (newborn testing)
-
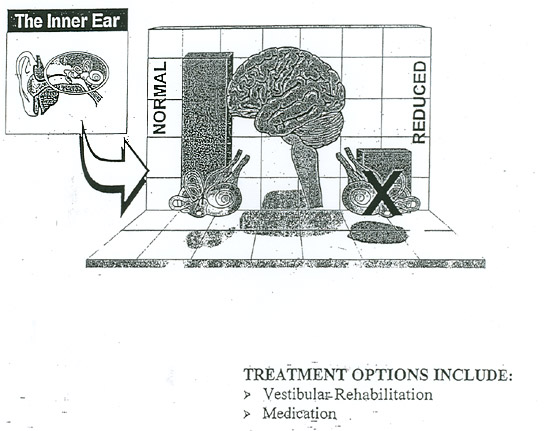
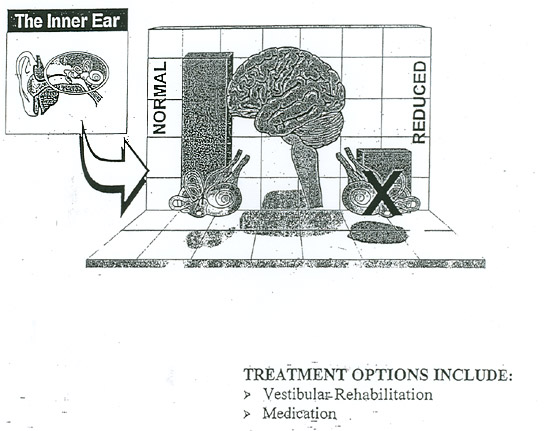
Vestibular Rehabilitation (balance and dizziness)
-
New Digital Hearing Aid Technology
To learn more about some of the specific conditions we treat, click on the links listed below:
|
|
Benign Paroxysmal Positional Vertigo (BPPV)
Have you ever rolled over in bed to kiss your spouse goodnight, turn off the alarm clock, or to toss "Fluffy" the cat, out of bed and then suddenly felt as though the world was spinning out of control? Well, you may have experienced the most common fonn of vertigo, known as Benign Paroxysmal Positional Vertigo. It is often referred to as BPPV.
This most common fonn of vertigo is prevalent in all age groups. By age seventy, fifty percent of all individuals will experience this frightening sense of falling, tumbling, or spinning at least once in their lives, In younger individuals, it may occur following medical conditions such as Meniere's disease, vestibular neuronitis, labyrinthitis, migraine, or after even a mild head trauma.
The sensation can be quite frightening. It can be strong-feeling like you're being pushed off a bridge, or being pulled down by a giant magnet. The condition itself is rarely dangerous or life threatening. However, the consequences of being acutely dizzy with such strong sensations of being out of control is what can really get you in trouble.
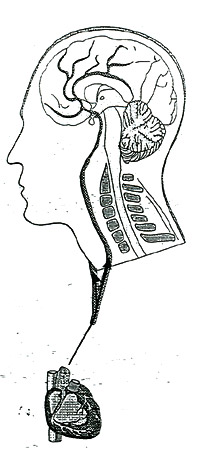
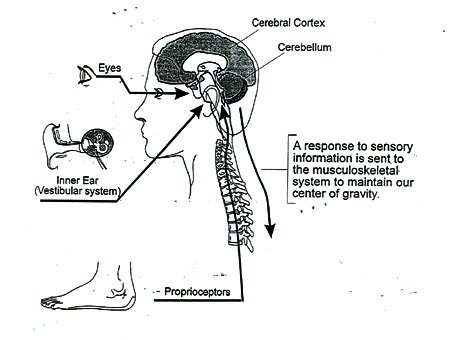
How the balance system works:
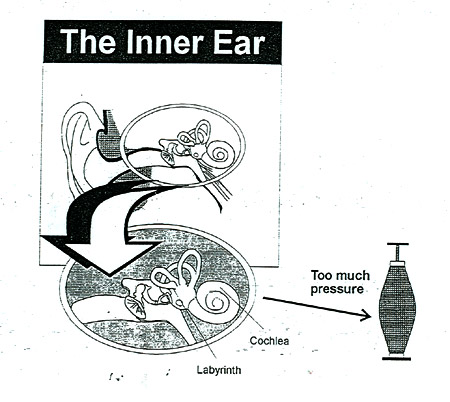
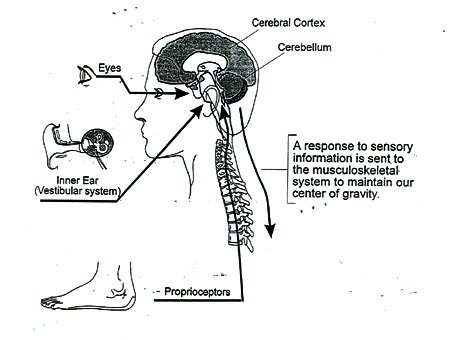
Most of us, when asked about the main function of the inner ear, would respond, "It is our sense of hearing". The correct answer is the primary function of the inner ear is equilibrium. Within the inner ear there are two distinct parts: the hearing portion, referred to as the cochlea; and the balance portion, which we call the vestibular system or labyrinth. The labyrinth is comprised of two portions. The undennost portion, referred to as the otolith system, is actually a gravity sensor, which tells our brain about the pull of gravity. This is made up of both the utricle and the saccule, an within these two structures are calcium carbonate crystals whose weight responds to the pull of gravity by resting on nerve endings that sends a signal to the brain about the force or pull of gravity. When astronauts travel into micro gravity, the lessening of the weight against the nerve endings will cause them to become "space sick". When tl],ey return to earth, the weight now pressing on the nerve endings causes them to be "land sick".
Why do we get positional vertigo?
Most of the time, this system works quite well. Any nonnal degeneration of these calcium carbonate crystals, also called otoconia, fall into the back semicircular canal, aptly named the posterior canal. The semicircular canals (the three balance canals), are designed to be velocity sensors and not gravity sensors. So, when the additional weight of the otoconia enters into these canals, it converts this velocity sensor into a gravity sensor. While our head is erect, seated, or standing, it may not cause difficulty when we look up however, or when we lie flat with our head completely back or rolled to one side, the debris, which is now in the back balance canal (the posterior canal), causes the nerve endings to be misdirected. This, in turn, causes the hallucination of rolling, spinning, or turning, which we term "vertigo". During this instance, if our eyes are open, our vision may seem blurred or the world around us may appear to be in a spin. This is because our inner ears are responsible for influencing eye movement.
The calcium carbonate needs to be in sufficient quantities where it becomes heavy enough to be able to push or move the nerve endings. We all have some amount of otoconia loose in our balance canals. The biochemistry of the human body is such that our bodies should normally absorb this calcium within hours, or certainly days, and it never gets to a point where it is heavy enough to cause dizziness symptoms. There are now some theories that the reason some individuals become symptomatic with BPPV their body's biochemistry is having difficulty with calcium absorption. This, of course, only a theory and is not intended to discourage the use of calcium, a critically important element in all organ functions, as well as necessary for our nervous system. It is just one of those odd things that seems to occur in some individuals.
Treatment:
The good news about BPPV is that for many people, the experience will not last more than a few days and it will seem to disappear as quickly as it came. For others, however, it may last for days, weeks, months, and even years. There is no medication that will treat this problem. Anti-motion medication such as mec1izine or Antivert may minimize the dizziness or accompanying nausea, but will not treat the problem itself.
In 1988, at the Paris Ear Institute, a French physiatrist, Alain Semont, along with a group of French ear, nose and throat physicians wrote a paper and presented a simple treatment, a five-minute physical therapy maneuver, which moved the debris to circulate through the long arm of the posterior canal and drop back into the utricle. Once the debris entered the utricle, ifthe patient did not return to the problem position for a day or two, the symptoms would resolve. The theory was that the biochemistry of the utricle, because it is a larger space, is different from that of the posterior canal~ and this allows the calcium carbonate to readily dissolve in the larger space, while it could not do so when in the smaller area of the posterior canal.
Since Semont's article, dozens of studies and methods of varying techniques from balance specialists around the world have been published. The treatments may be referred to a Semont Liberatory Maneuver, Epley Repositioning Maneuver, Gans Repositioning Maneuver, or simply Canalith Repositioning Maneuver. These treatments, all basically achieve the same thing, but require the patient to be moved into slightly different head or body positions. The treatments are usually performed by an audiologist.
It is possible that other canals, predominantly the side canals (referred to as the horizontal canals) may also contain some trapped debris. These canals require other fonns of treatment, which also have been written about for many years, and may include treatments known as Appiani, Casani, or Bar-b-que. Roll. Research has not shown that one treatment is better than the other, but are decided upon by the individual clinician or therapist based on the nature of the problem, as well as any physical imitations or restrictions such as the range of motion of your neck, and any back or shoulder problems. The treatment is very simple, and may range anywhere from three to ten minutes to perform, depending upon the variation.
It has been customary to ask the patient not to lie flat for at least one or two nights following treatment, and to perhaps avoid lying on the side of the affected ear for several nights. Sometimes patients have been provided with a soft cervical collar as a friendly reminder to help them to keep their head from tipping or moving. Recent studies suggest, however, that some of these restrictions may not be necessary, but the jury is still out on this, In the meantime, it is likely that if you find you have BPPV and seek treatment, your clinician will ask you to restrict some of your daily activities or your head positions. There are a number of excellent web sites that provide additional infonnation concerning the diagnosis and treatment of BPPV.
A word of caution: Although some web or information sites may show you the treatment diagrams, I am not in favor of having patients self-perfonn them. The reason being, it is very important that a proper diagnosis be made before treatment starts! There is a number of other rather serious medical conditions that share some of the same symptoms and may mimic BPPV. Positional vertigo can be caused by such other disorders as Arnold Chiari malfonnations, vascular loop, subdural hematoma, or posterior fossa cyst. Likewise, if a patient has cervico-spinal problems where there is compression of blood flow through the vertebral artery, it is possible that if they are not properly screened and were to hyper-extend and rotate their neck improperly, a stroke could result.
The purpose of these comments if not to unnecessarily frighten anyone, but to further confirm that although BPPV is not a serious, condition and can be treated quite readily with no discomfort or special equipment, there can be a number of other medical conditions, which are far more serious, which may need to be completely differentiate by a trained professional.
Summary:
In summary, you can learn more about BPPV from various websites, but most importantly, recognize the fact that if you indeed are diagnosed with this condition, you do not have to learn to live with the problem because it can be treated simply and quickly.
|
|
Tinnitus
WHAT IS TINNITUS? Tinnitus represents one of the most elusive mysteries facing audiologists and other hearing health care professionals. It refers to an auditor perception not directly produced by an external sound. Tinnitus commonly described as a "hissing, roaring or ringing". It can range tTom high pitch to low pitch, consist of multiple tones or sound like noise (having no tonal quality at all). Tinnitus may be constant, pulsed or intermittent. It may begin suddenly, or ma~ come on gradually. It can be perceived in one ear, both ears, or in the head.
WHO HAS TINNITUS? As many as 50 million adults experience tinnitus, with more than 10 million seeking help for the condition. Because tinnitus, like pain, is subjective, two individuals may report similar tinnitus characteristics yet be affected in significantly different ways. The severity of tinnitus and how it affects one's life is largely influenced by the individual's reaction to the tinnitus. Many tinnitus sufferers report interference with sleep, concentration, and attention to detail. Some are depressed and anxious and may report additional problems at work or at home that compound the distress caused by tinnitus. Many people with tinnitus also suffer tTom hyperacusis, an inability to tolerate even moderate level sounds. Most tinnitus patients report a relationship between tinnitus perception and stress. The onset of tinnitus often concides with a change (emotional, physical or social) in one's life situation. Tinnitus has both physiological and psychological component.
WHAT CAUSES TINNITUS? The exact mechanism underlying tinnitus is unknown. It is likely that there are many mechanisms. Some of the potential causes are:
-
Disorders in the outer ear such as: ear wax (cerumen), hair or a foreign body touching the eardrum;
-
Disorders in the middle ear such as: vascular abnormalities, infection, otosclerosis, muscle spasms, Eustachian tube dysfunction, benign tumors;
-
Disorders in the inner ear such as: sensorineural (nerve) damage due to noise exposure, presbycusis (hearing loss tTom aging), labyrinthitis (inner ear infection), Meniere's disease (associated with hearing loss and dizziness);
-
Temporary effects of high dosages of medications such as anti-inflammatories (including aspirin, ibuprofen, and quinine) certain sedatives and antidepressants; possible permanent effects from certain antibiotics and chemotherapeutic agents;
-
Systemic disorders such as high or low blood pressure, anemia, diabetes, thyroid dysfunction, glucose metabolism abnormalities, vascular disorders, acoustic tumprs, head or neck aneurisms, hormonal changes;
-
Trauma to the head or neck, cervical (neck) problems, temporomandibular Gaw joint) misalignment.
WHAT TREATMENTS ARE AVAILABLE FOR THE TINNITUS PATIENT? Because tinnitus may be symptomatic of a treatable disease, it is important to try to identify and resolve a cause before deciding on the management approach.
A variety of tinnitus management procedures (listed below in alphabetical order) are available. None are universal cures, but most tinnitus sufferers can find varying degrees of relief from one or a combination ofthe following procedures:
COUNSELING: Counseling should be part of any treatment plan. There are many forms of counseling. Usually, a trained professional will attempt to help the patient deal with the stress, distress, and distraction associated with tinnitus. One form of counseling that is often employed is cognitive-behavioral therapy, a procedure that is also used for patients suffering from chronic pain. The objective of this approach is to help individuals identify and correct maladaptive behaviors and irrational beliefs that maintain their adverse reaction to the tinnitus.
HEARING AIDS: Amplification is among the most effective tools for providing relief from tinnitus. Hearing aids may help by amplifying background sounds that reduce the loudness of the tinnitus or even mask it. In addition, they may help by relieving stress associated with the adverse impact of hearing loss on communication abilities.
MASKING: The use of an externally produced sound to either cover up, inhibit or alter production of tinnitus can offer temporary, partial or complete relief for some tinnitus sufferers. There are several methods of providing masking; including tinnitus maskers (ear level electronic sound-producing devices housed in a hearing aid case), tinnitus instruments (combination hearing aids and tinnitus maskers), tabletop bedside sound generators or hearing aids. CDs and tapes that provide various sounds also may help mask til1l1itus. These can be used with either speakers or headphones.
MEDICATIONS: There is no single medication that works for all tinnitus patients. Some antidepressants and anti-anxiety medications address the problems associated with tinnitus and have proven helpful for certain patients. Always consult your physician concerning any drug or combination of medications you may be considering.
STRESS MANAGEMENT, RELAXATION AND BIOFEEDBACK:These are examples of various techniques used to help one cope with the stress of tinnitus. The close relationship between stress and tinnitus disturbance underscores and logic when trying to manage tinnitus.
SUPPORT/EDUCATION GROUPS: Groups offer a forum for sharing experiences and useful strategies with others. They may also offer emotional support to patients.
TINNITUS HABITUATION (RE-TRAINING): This technique is based on the principles of neural plasticity (brain re-wiring). The two components of this method are directive counseling (education) and sound therapy. Some experts believe that a conditioned response is created within the central auditory nervous system, and that with proper counseling, education and understanding, the brain can relearn a pattern that removes the fear and de-emphasizes the importance of the tinnitus. For the sound therapy component, a wide band sound is presented via hearing aid type devices at a soft enough level that the brain perceives both the sound from the devices and the tinnitus. Eventually, the brain may relearn a pattern that will de-emphasize the importance of the tinnitus.
ALTERNATE APPROACHES: There is no scientific data showing consistent benefit from approaches such as hypnosis, acupuncture, homeopathy, vitamin supplements or chiropractic manipulation, though anecdotal reports indicate benefit for some patients. It should be exercised and your physician should be kept appraised of any substances you are using.
WHAT CAN YOU DO TO MINIMIZE TINNITUS?
-
Avoid loud noises
-
Wear proper ear protection in high noise areas
-
Control stress . Avoid fatigue . Learn to relax
-
Maintain good nutrition; certain disorders may be helped by lowering salt intake
-
Reduce or eliminate stimulants such as caffeine or alcohol
-
Exercise
-
Educate yourself about tinnitus
|
|
|
Vestibulopathy
- A change or reduction in the output of one or both of the balance portions of the inner ear (vestibular system) may be caused by infection, illness, trauma, or simply the natural aging process. Symptoms may.include: positional vertigo, a sense of motion with rapid head movement, or a visually provoked motion intolerance.
|
|
Dysequilibrium
- A loss of balance which may be caused by changes from any one or all three of the primary equilibrium sensory systems, or the central relay system in the brain. Sympt6oms may include a loss of sure footedness, difficulty walking or moving about without touching walls or objects, and trouble changing surfaces, e.g. tile to carpeting.
|
|
Central Auditory Processing Disorders (CAPD's)
- What are central auditory processing disorders (CAPDs)?
CAPDs are often characterized by a child having difficulty understanding speech or instructions in the presence of normal hearing sensitivity. They usually are noticed when the child is in an atmosphere of sensory overload. Too much is happening around the child and so the child cannot "process" the same information that other children process. This also can occur when the "redundancy" of the auditory information is reduced: when speakers cannot be seen, when the normal frequency content of speech is reduced, or especially when an ear infection produces a mild and temporary hearing loss.
How is CAPD diagnosed?
There are a number of tests that are used to diagnose the presence of CAPD. Usually, these tests require that a child repeat words, phrases, or tonal sequences when the test signal is presented in the at the same time as a competing messages (background noise) or when the signal has been filtered to eliminate some frequencies from the normal spectral content. Sometimes, children are asked to repeat separate but simultaneous messages directed to each ear.
|
The use of an auditory trainer allows the child to focus his/her attention on the teacher and to reduce the interference of background noise.
|
The child's scores on the tests are compared to normative scores that have been gathered from children of the same age who do not have CAPD.
What strategies can be used to help a child with CAPD?
Most of the strategies listed below are designed to maximize the child's strengths and to not overload the child. Some strategies may work better than others. Please be flexible and discover which strategies are more appropriate for your child.
-
Place your child in classroom settings that avoid noisy or reverberant environments. Avoid open classroom placement.
-
Preferentially seat your child near the area that the teacher spends most of his/her time.
-
Teach your child to use visual information: look and listen.
-
Gain your child's attention before giving auditory instructions. You might call your child's name, cue your child by saying "listen" or "ready" before giving assignments.
-
Check your child's comprehension of auditory information before moving on to another topic.
-
Restate important information. When repeating, try phrasing the information in a different way.
-
Teach strategies that compensate for weak areas. For instance, assignments that are given orally could be checked with the teacher at the end of the class period.
-
Teach listening skills. For instance, your child should wait until instructions are completed by the teacher before beginning a task.
-
Give your child enough time to think and to respond to auditory instructions or questions.
-
Give your child information in smaller packets. Rather than giving a multistage instructions, provide instructions in "sound bites".
-
Allow a "buddy" system with another child so that your child can check on homework assignments or other instructions.
Will hearing aids help a child with CAPD?
Hearing aids would only be recommended if the child with CAPD also has a hearing loss that is suitable for the use of hearing aids. If the child does not have a hearing loss, then it is likely that hearing aids would probably worsen the child's situation by introducing overly loud sound.
Auditory trainers, which are a form of Assistive Listening Devices, can be useful for children with CAPD. The teacher wears a microphone/transmitter while the child wears a receiver/headset. The use of an auditory trainer allows the child to focus his/her attention on the teacher and to reduce the interference of background noise. Children who wear hearing aids also can make use of this technology. Many hearing aids have the ability to be modified for direct auditory input. The input comes from the receiver of an auditory trainer or may be self contained. Neck loops also can be used in combination with the telecoil circuit in the hearing aid.
Behaviors of Children with CAPD
-
Says “huh” or “what” frequently
-
Inconsistent responses to auditory stimuli
-
Often misunderstands what is said
-
Requests that information be repeated
-
Poor auditory attention
-
Exhibits extreme distractibility
-
Difficulty following oral instructions
-
Difficulty listening in the presence of background noise
-
Difficulty with phonics and speech sound discrimination
-
Poor auditory memory span
-
Poor sequencing skills
-
Poor receptive and expressive language skills
-
Slow or delayed response to verbal requests and instructions
-
Reading, spelling and other academic problems
-
Learns poorly through the auditory channel
-
Exhibits behavior problems
Academic symptoms of children with CAPD
Auditory Discrimination Deficit:
Child will have trouble understanding verbal directions; will make errors in repeating words and directions; will substitute words, numbers, etc. Will have difficulty learning sounds for letters, letter names, etc. May have trouble learning names of people, places and things.
Auditory Memory Deficit:
Will have trouble recalling names of things, letters, words, numbers, etc. May not consistently remember addresses, phone numbers, etc. from day to day. May not remember how to pronounce letters and words.
Auditory Association Deficit:
May have trouble learning sounds of letters and letter names, individual words with categories, etc. May not be able to follow verbal directions, conceptualize the concepts of words, numbers, etc. May have difficulty classifying objects and ideas presented verbally.
Auditory - Visual Association Deficit:
This skill requires functioning of lower level skills plus relating a visual symbol with a sound for that symbol. This skill is the essence of word recognition. Subjects with this deficit will have trouble recognizing and naming letters, words, numbers, etc. May be able to write what is read, speak what is heard, but will have trouble speaking what is read, or writing what is heard. This manifests as note taking problems in school.
|
|
|
Hearing & Balance Disorders
|
|
Hydrops and Meniere's Diet Suggestions
- The fluid-filled hearing and balance structures of the inner ear normally function independent of the body's overall fluid/blood system. In a normal inner ear, the fluid is maintained at a constant volume and contains specific concentrations of sodium, potassium, chloride, and other electrolytes. This fluid bathes the sensory cells of the inner ear and allows them to function normally.
With injury or degeneration of the inner ear structures, independent control may be lost, and the volume and concentration of the inner ear fluid fluctuate with changes in the body's fluid/blood. This fluctuation causes the symptoms of hydrops -- pressure or fullness in the ears, tinnitus (ringing in the ears), hearing loss, dizziness and imbalance.
Diet and Dizziness
Your inner ear fluid is influenced by certain substances in your blood and other body fluids. For instance, when you eat foods that are high in salt or sugar, your blood level concentration of salt or sugar increases, and this, in turn, will affect the concentration of substances in your inner ear.
People with certain balance disorders must control the amount of salt and sugar that is added to food. You must also become aware of the hidden salts and sugars that foods contain. Limiting or eliminating your use of caffeine and alcohol will also help reduce symptoms of dizziness and ringing in the ears.
Dietary Goals
The overall goal is to provide stable body fluid/blood levels so that secondary fluctuations in inner ear fluid can be avoided. The following steps will help you achieve this goal. 1. Distribute your food and fluid intake evenly throughout the day and from day to day. Eat approximately the same amount of food at each meal, and do not skip meals. If you eat snacks, have them at regular times.
2. Avoid taking in foods or fluids that have a high salt or sugar content. High salt or sugar levels in the diet result in fluctuations in the inner ear fluid pressure and may increase your symptoms. Aim for a diet high in fresh fruits, vegetables, and whole grains, and low in canned, frozen, or processed foods.
3. Drink adequate amounts of fluid daily. This should include water, milk, and low-sugar fruit juices (for example, cranberry). Coffee, tea, and soft drinks should not be counted as a part of this intake. Try to anticipate fluid loss that will occur with exercise or heat, and replace these fluids before they are lost.
4. Avoid caffeine-containing fluids and foods (such as coffee, tea, and chocolate). Caffeine is a diuretic that causes excessive urinary loss of fluids. Caffeine also has stimulant properties that may make your symptoms worse.
5. Limit or eliminate your alcohol intake. Alcohol can affect the inner ear directly, changing the volume and concentration of the inner ear fluid and increasing symptoms.
6. Avoid foods containing MSG (monosodium glutamate). This is often present in pre-packaged food products and in Chinese food. It may increase symptoms in some patients.
Drug Considerations
1. Avoid aspirin and medications that contain aspirin. These can increase tinnitus and dizziness.
2. Avoid caffeine-containing medications.
3. Pay attention to the content of all over-the-counter medications as well as drugs prescribed by physicians for other problems. Some may increase your symptoms.
4. Avoid cigarettes. The nicotine present in cigarettes constricts blood vessels and will decrease the blood supply to the inner ear, making your symptoms worse.
|
|
Serenade
- The Serenade system consists of a handheld device, earphones, and proprietary treatment sounds that research has suggested may address the underlying neurological cause of tinnitus. This novel technology is simple to use and customized specifically to your tinnitus. It may be used to seek immediate relief, as well as long term benefit when used as part of an ongoing tinnitus treatment program. After an audiologist evaluates your tinnitus, your Serenade device is programmed to play the sounds most likely to be effective for you.
Features of Serenade®:
-
Unlike other approaches, this treatment is customized to your specific tinnitus.
-
Includes 4 separate sound tracks so you can select the one that works best for you, day or night.
-
New treatment sounds known as S-Tones® were developed by independent leading university hearing experts and only recently commercialized.
-
This technology is based on advanced research and solid science, and is FDA cleared.
-
The device is small, portable, and easy to use.
-
Includes SleepAssist – a 60 minute, auto-off timer to help you fall asleep.
-
Independent left and right volume controls offer maximum flexibility, comfort and customization.
Ask us about Serenade and whether it may be right for you.
For more information about Serenade®, ask your audiologist or visit www.soundcure.com.
Did You Know?
-
1 in 10 adult Americans suffer from tinnitus.
-
Many patients are not offered treatment and are told to “just live with it.”
-
Tinnitus can almost always be treated and its symptoms improved.
|
|
Board Certified & Licensed
"Care, Quality and Commitment"
    
|
|
|
 (409) 832-0999
(409) 832-0999